Introduction
Body Mass Index (BMI) has long been a standard tool in healthcare settings to assess an individual’s body weight relative to their height. However, its efficacy and accuracy have been subjects of debate among healthcare professionals. As a dietitian, I often encounter patients who are either overly concerned or dismissive of their BMI. This blog post aims to explore the pros and cons of using BMI as a tool to identify health risks, delve into its history, discuss its creation, and provide insights on how it should be used properly in healthcare settings.
The History and Creation of BMI
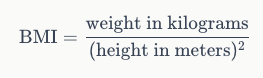
The concept of BMI was developed by Adolph Quetelet, a Belgian mathematician, astronomer, and statistician, in the early 19th century. Quetelet was interested in defining the characteristics of the “average man” and developed the Quetelet Index, which we now know as BMI. The formula for BMI is straightforward:
BMI gained widespread acceptance in the medical community in the 20th century. It was popularised by Ancel Keys, a physiologist who conducted extensive research on the relationship between body weight and health. Keys found that BMI was a simple and effective way to categorise individuals based on their weight and height, making it a useful tool for identifying potential health risks.
Why Do We Use BMI?
One of the primary advantages of BMI is its simplicity. The calculation requires only two measurements: weight and height, which makes it an accessible tool for both healthcare professionals and the general public. BMI can be quickly calculated and interpreted, providing an immediate snapshot of an individual’s weight status. Generally, it is also pretty accurate for the overall populations health; we know that individuals who are at a BMI of above 30kg/m2 are more likely to develop obesity related conditions, and so we can utilise it across the general population to identify those who are more at risk of conditions such as type 2 diabetes, cancers and cardiovascular disease.
Because of this, BMI is particularly useful for population-level screening. It allows public health officials to assess the prevalence of underweight, normal weight, overweight, and obesity within large groups. This information is crucial for developing public health policies and interventions aimed at addressing weight-related health issues.
The Cons of Using BMI
Perhaps the most significant criticisms of BMI is its lack of individual specificity. BMI does not account for differences in body composition, such as muscle mass, bone density, and fat distribution. For example, a bodybuilder with a high muscle mass may have a high BMI but a low percentage of body fat, which does not necessarily indicate poor health, and as such, they would be flagged at being at risk for conditions and told to lose weight when that is really not an appropriate intervention.
Unfortunately, this nuance doesn’t seem to have made its way into public sector healthcare. Many treatments (such as fertility treatment) have a hard BMI cut off, which leads to many people not getting the healthcare they need because the provider does not add nuance to the equation.
Another (often rather frustrating thing) about BMI is that it often does not consider ethnic and gender variations in body composition. Different ethnic groups have varying levels of body fat at the same BMI, and men and women naturally have different body fat distributions. As the initial research on BMI was done on white men, the calculations cannot be considered to be inclusive for all other ethnicities and genders. This can lead to misclassifications and inaccurate assessments of health risks. Whilst, yes, there are now different cut offs for different ethnicities (for example, South Asian men are considered overweight at a BMI of 23kg/m2 and obese at a BMI of 25kg/m2, compared to 25kg/m2 for overweight and 30kg/m2 for obese in white populations), there hasn’t been specific research into this at this stage to verify that these cut offs are appropriate.
BMI also focuses solely on weight and height, ignoring other critical factors that contribute to overall health, such as diet, physical activity, genetics, and metabolic health. Many individuals can have a higher BMI, but much healthier lifestyle patterns than others with a lower BMI, making them overall at a lower risk of disease. Relying solely on BMI can overlook these important aspects and provide an incomplete picture of an individual’s health status.
Proper Use of BMI in Healthcare Settings
BMI should only be used as a complementary tool rather than a standalone diagnostic measure. Healthcare professionals should combine BMI with other assessments, such as waist circumference, body fat percentage, and blood pressure, as well as a visual assessment of body composition, food and lifestyle diaries, to gain a more comprehensive understanding of an individual’s health.
Healthcare professionals should also do their part on educating patients about the limitations of BMI and its role as part of a broader health assessment is crucial. We should use BMI as a starting point for discussions about healthy lifestyle choices, including diet and physical activity, rather than as a definitive measure of health.
In conclusion, while BMI is a useful and accessible tool for assessing weight status and identifying potential health risks, it is not without its limitations. As a dietitian, I advocate for a balanced approach that uses BMI as part of a comprehensive health assessment. By understanding its history, acknowledging its pros and cons, and using it appropriately in healthcare settings, we can ensure that BMI serves as a valuable tool in promoting overall health and well-being.
Remember, BMI is just one piece of the puzzle. A holistic approach to health that considers various factors will always provide the most accurate and beneficial insights for individuals.