Prader-Willi Syndrome (PWS) is a complex, rare genetic disorder that affects multiple systems in the body, leading to a variety of physical, cognitive, and behavioural challenges. While every individual with PWS is unique, the condition is marked by a combination of developmental delays, hormonal imbalances, and significant difficulties with appetite regulation.
What is Prader-Willi Syndrome?
Click here for a video summary of what Prader-Willi syndrome is.
Prader-Willi Syndrome is a genetic disorder that occurs due to the loss or malfunction of genes on chromosome 15. This syndrome is typically caused by a deletion in the paternal copy of chromosome 15 or, in rarer cases, an uniparental disomy, where two copies of chromosome 15 come from the mother and none from the father. Either way this genetic anomaly significantly impacts the lives of those with PWS. It is a very rare condition; typically affecting between 1 in 10,000 and 1 in 25,000 newborns, and as it is genetic, it cannot be developed later in life, nor can someone who is born with it recover from it.
There are 3 primary areas of health and development which are affected by PWS:
| Neurocognitive | Hormonal | Behavioural |
| People with PWS often have a learning disability, although this can vary in severity depending on the person. PWS also causes changes in the brain structure, which can impact cognition. | People with PWS have significantly changed hormonal responses. Many hormones, including those involved in appetite regulation, hunger and satiety do not work as they should. | Many people with PWS experience compulsive behaviours, anxiety symptoms and may also have behavioural issues around food. |
How does this impact what they eat?
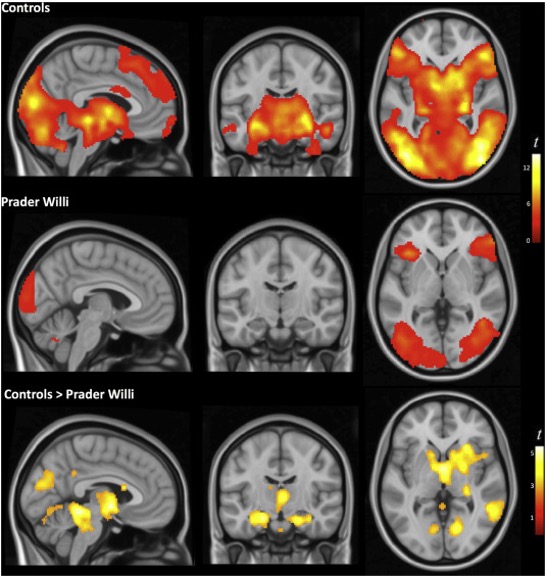
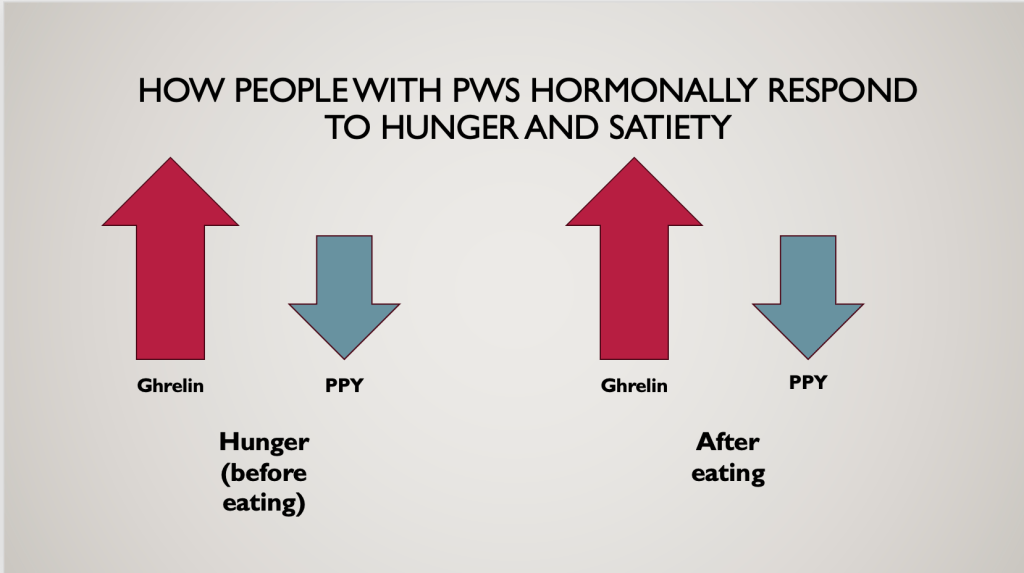
People with PWS have altered brain functions when it comes to food. When they eat, their food activation (red) areas are stimulated, and the more they eat, the more the areas are stimulated. This differs to someone without PWS, who would have their food inhibitory (yellow) areas stimulated, to get them to stop eating. Essentially, the more they eat, the more they crave, and this effect is worsened when they eat ultra-processed, highly palatable foods. This image shows the impact of eating a non-palatable food on the brains of people with and without PWS.
Blanco-Hinojo et al (2019)
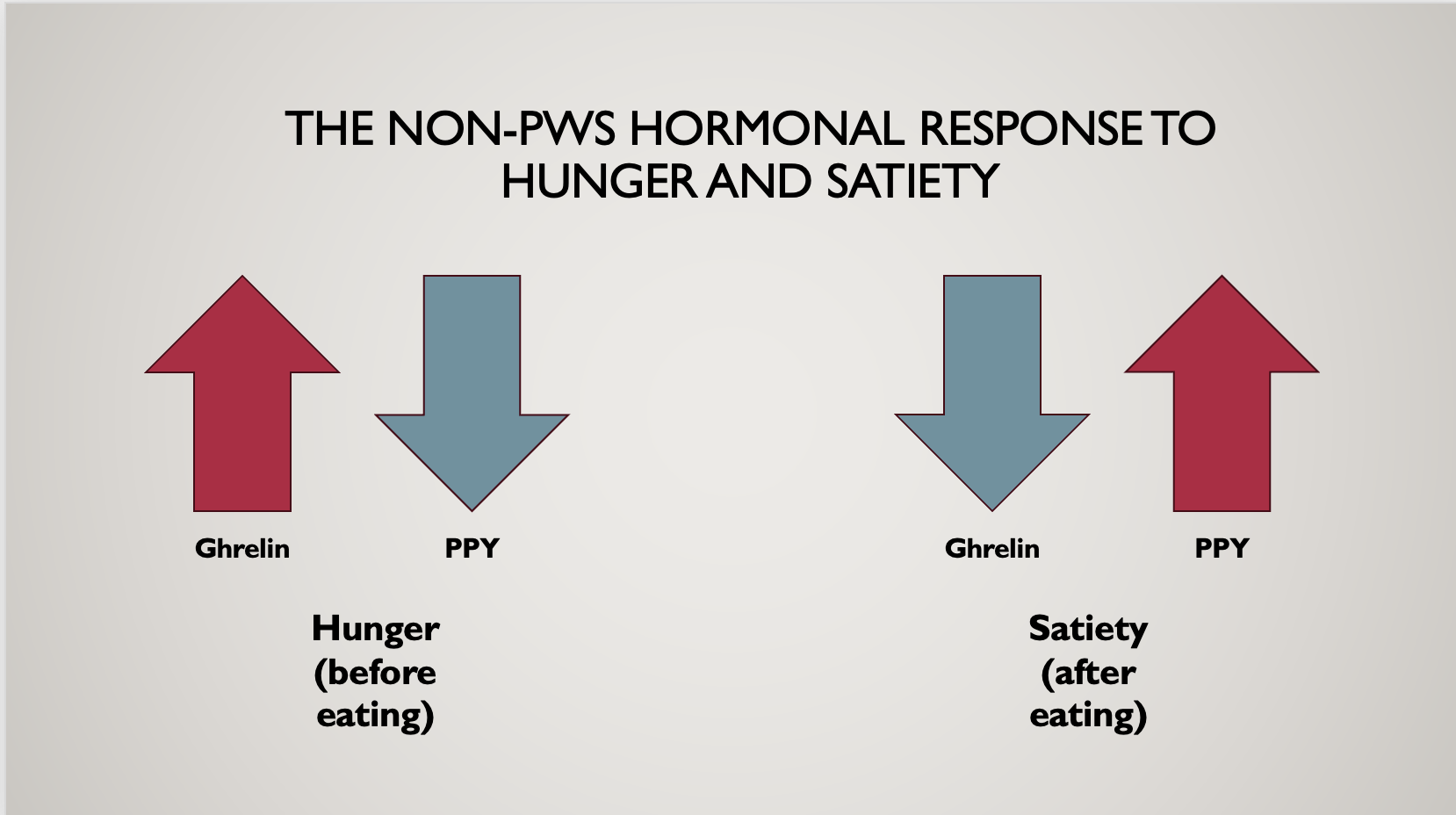
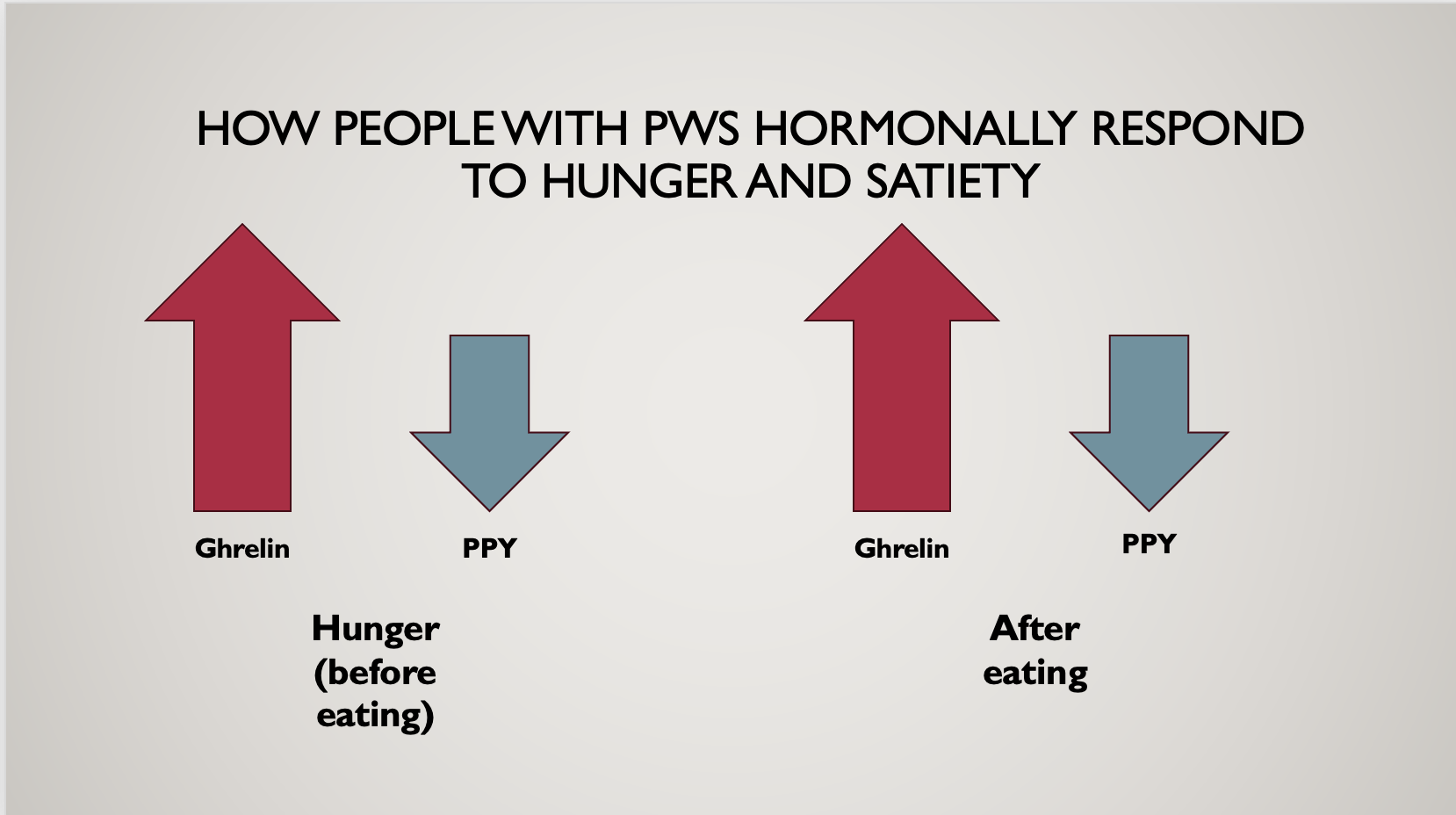
Every person has hormones within their body which help to regulate our feelings of hunger and fullness.
- Ghrelin- this is the hunger hormone. It increases when we are hungry and decreases when we are full.
- Pancreatic Polypeptide (PPY) and leptin- these are the fullness hormones. These should increase when we are eating to tell us when we are full, and will decrease again when we are hungry.
You can see in the pictures above, that in someone without PWS, these hormones function normally- ghrelin increases when we are hungry and PPY increases when we are full. However, for people with PWS, these don’t function properly.
People with PWS produce more ghrelin a their baseline, meaning they are perpetually more hungry than the average person. When they eat, their ghrelin production doesn’t stop, so they remain hungry even if their stomach is full to bursting. They also do not produce enough PPY, meaning they don’t have the signal to tell them to stop eating either.
The impact of hormonal and neurocognitive changes on food intake
Because the brains and hormone production in people with PWS is so different to someone without PWS, it can be hard for us to comprehend the impact this has on their psyche. Essentially, someone with PWS is constantly feeling starving. Very little changes this feeling, even when they have eaten pounds and pounds of food. Understandably, this can cause behaviours around food which can be difficult to understand; hoarding food, eating food items which are not prepared into typically edible food (such as bags of sugar or sticks of butter), raiding cupboards and fridges, and potentially behavioural issues when denied food.
The other issue: body composition
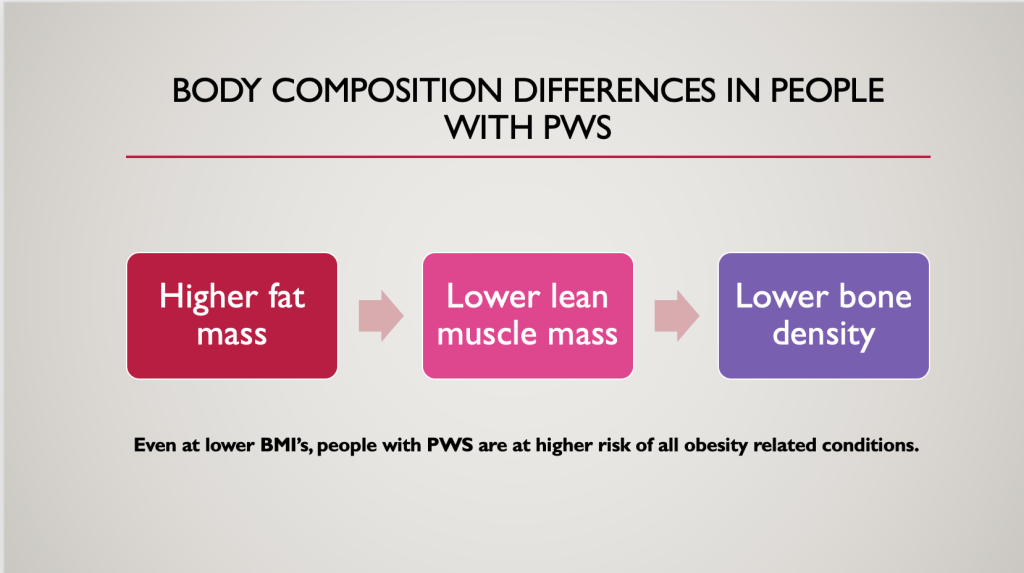
People with PWS have a double whammy when it comes to managing their weight; not only do they have to deal with insatiable hunger, they also have differences in body composition which means that they are at a higher risk for conditions such as cardiovascular disease and type 2 diabetes than the average person at a lower weight.
Higher fat mass, lower lean muscle mass and lower bone density, caused by reduced hormone production (of growth hormone and adiponectin specifically) mean that they will have a higher body fat % which tends to be around the middle, increasing visceral fat (fat around the organs) and therefore making them more likely to have health conditions.
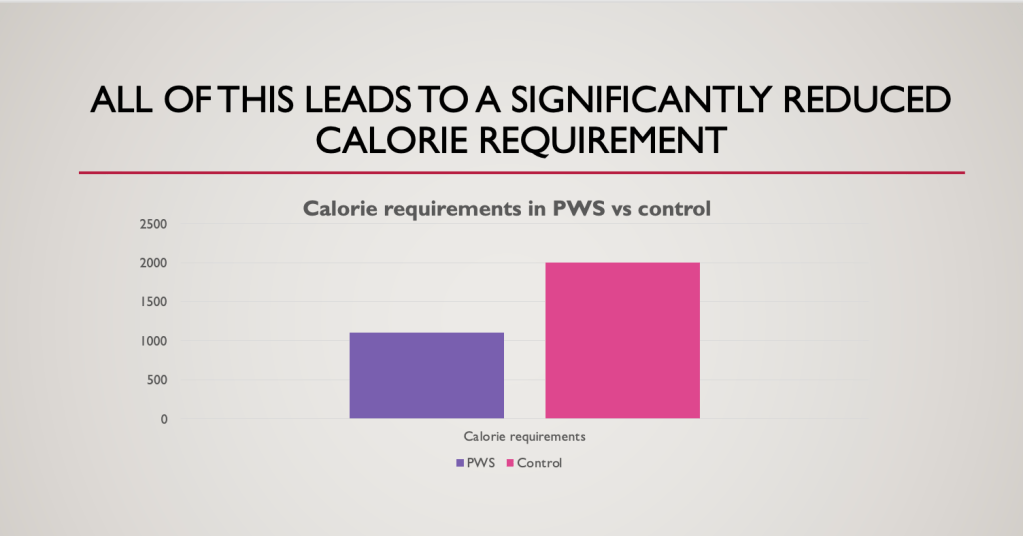
The other issue with a higher fat mass and less lean muscle mass is that fat mass, whilst not totally metabolically inactive, does not burn nearly as many calories per kilogramme as muscle mass does. Therefore, their calorie requirements are often significantly lower than the average persons.
Whilst there are very few studies on the calorie requirements of those with PWS, the general dietetic consensus is that they require 50-75% of the calories that an average adult of the same gender, height and activity level would require.
As a dietitian, I would calculate caloric requirements both by taking 50-75% of the BMR of a person without PWS and/or by using the formula of ~10kcals/ cm height for weight maintenance/ 6-8kcals/cm height for weight loss and finding the average. Therefore, for a 155cm woman, a calorie requirement of ~1,085kcals/day for weight loss would be appropriate.
Obviously the big problem is that even for us, without the ultra strong desire to eat that someone with PWS has, such a small amount of calories would be very difficult to stick to. Combine this with the hyperphagia and the constant feeling of starvation, this is very difficult to achieve in practice.
Impact on Health: present and future challenges
The combination of hormonal differences, neurocognitive differences, and behavioural concerns creates a complex medical picture for individuals with Prader-Willi Syndrome. These challenges impact both short-term and long-term health outcomes.
- Obesity-related Health Risks: As mentioned, one of the most immediate health risks for individuals with PWS is obesity, which can lead to other complications like diabetes, high blood pressure, heart disease and joint problems. Added to the fact that they often develop these conditions at a lower weight than the average person, it is vital weight is strictly maintained as much as possible to reduce the impact of these in the future.
- Endocrine Issues: Growth hormone therapy can improve some aspects of physical health, and other hormonal therapies may also help improve outcomes for people with PWS. This is individual, however, and needs to be discussed with medical professionals.
How dietitians can help people with Prader-Willi Syndrome
As a dietitian, I can play a pivotal role in the care of people with Prader-Willi Syndrome. Providing practical advice on how to manage the significant appetite and keep weight at a steady and stable level is vital for the health of the person with PWS, and can help prevent health conditions developing further down the line.
- Calorie restriction- whilst it may be tempting to think “it won’t hurt for them to have a little more at dinner or another 100 kcal chocolate bar”, for someone with PWS the impact that has is far more exaggerated than it would be for someone without it. For people who already have such low calorie requirements, it is vital to avoid giving into their cheeky and charming ways, as it can have a huge impact on their total daily calorie intake. You must be as strict and accurate as possible to ensure their calorie intakes are at the appropriate amount. A dietitian can help you identify what the appropriate calorie intake is for the person, as well as provide strategies to help you achieve this.
- Avoidance of ultra-palatable foods- foods high in fat, sugar and salt not only have a poor impact on overall health, but also will send those food activation centres haywire. If someone with PWS has a diet high in these foods, their cravings and hunger will be significantly stronger, and it can become harder to say no. A dietitian can give you practical advice on swaps you can make which can be lower in calorie and higher in nutrition to reduce the impact of this.
- Meal plans and structure around meals- It is key to have a meal plan that is produced every week with the person with PWS, so it can be referred to if they ask for food outside of meal times, and so they know that food will be coming soon. This can help reduce behaviours around food, particularly if you have to deny them something. A dietitian can help you find a meal plan which will work for you and the person you care for, and getting the person with PWS involved so they feel they have support and a say in what they are going to be eating.
- Environmental changes- locks on cupboards, fridges and banning from the kitchen may be needed for someone with PWS, but a dietitian can identify what would be appropriate for them.
Should you feel your loved one requires some help with managing their nutritional intake with Prader-Willi Syndrome, don’t despair! There are many dietitians, including myself, who are trained to help manage this condition. Get in touch today to see how we can help you.